Standard tests
Dry eye is caused by multiple factors and its diagnosis can involve various different examinations, including the following standard tests:

Questionnaire
There are several questionnaires used to assess the severity of dry eye and its impact on patients’ quality of life, including DEQ-5 (Dry Eye Questionnaire), OSDI (Ocular Surface Disease Index) and SPEED (Standard Patient Evaluation of Eye Dryness).
Clinical analysis
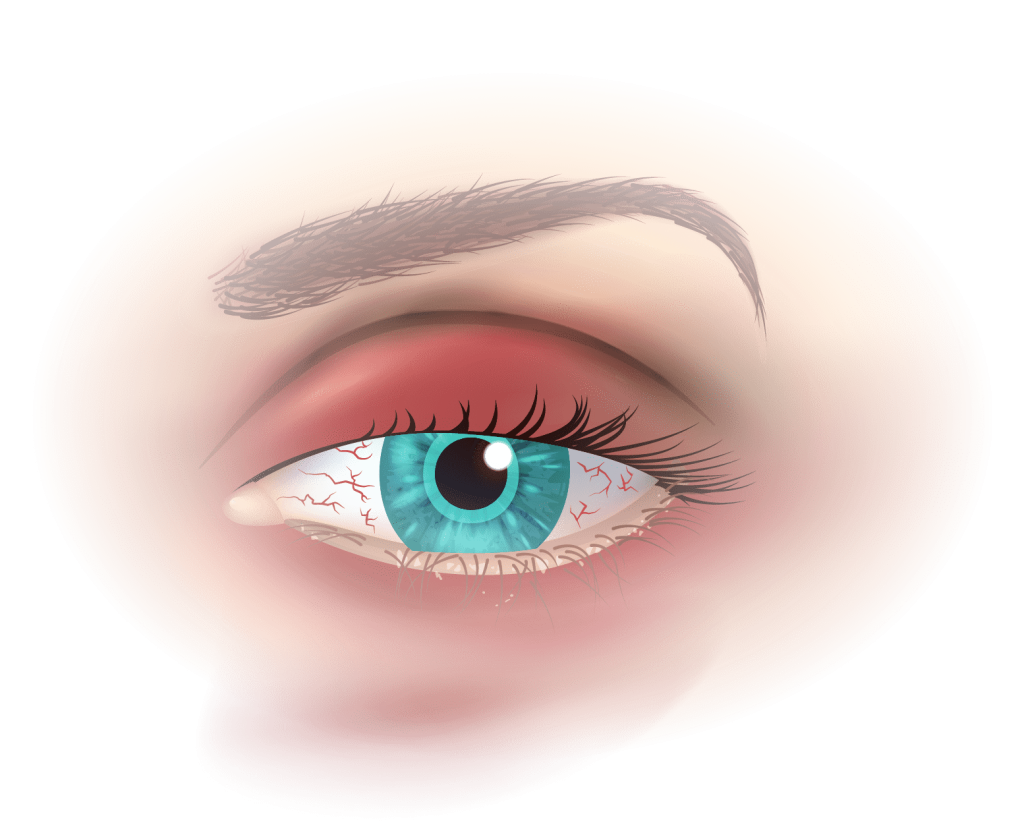
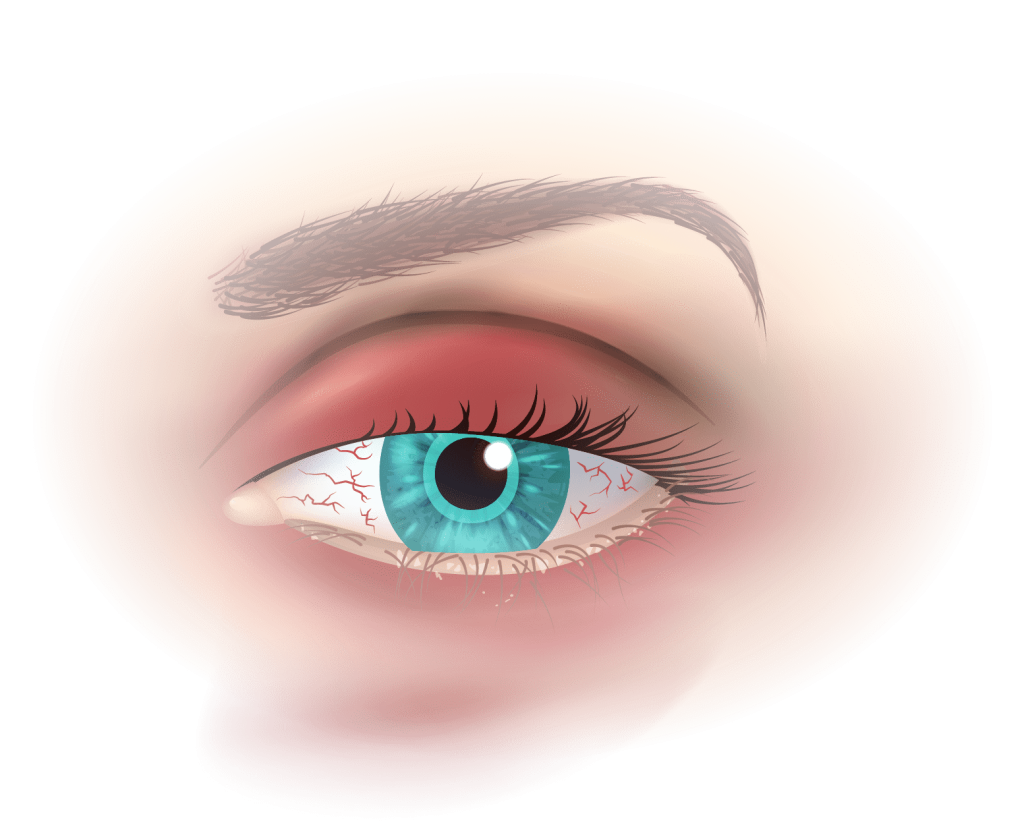
It is important to assess the appearance of the skin (for rosacea, eczema, psoriasis, seborrhoeic dermatitis), the anatomy of the eyelids, the appearance of the eyelashes, and blinking frequency.
Schirmer’s test
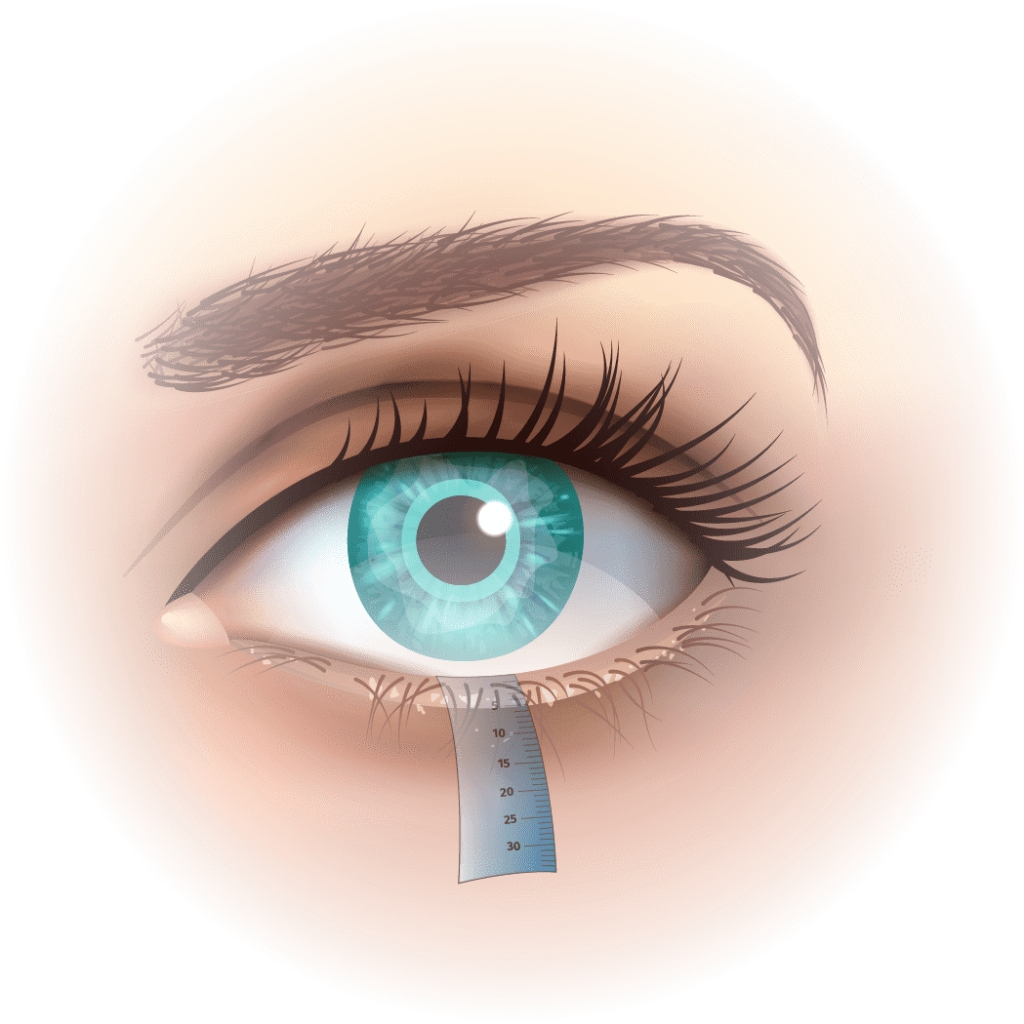
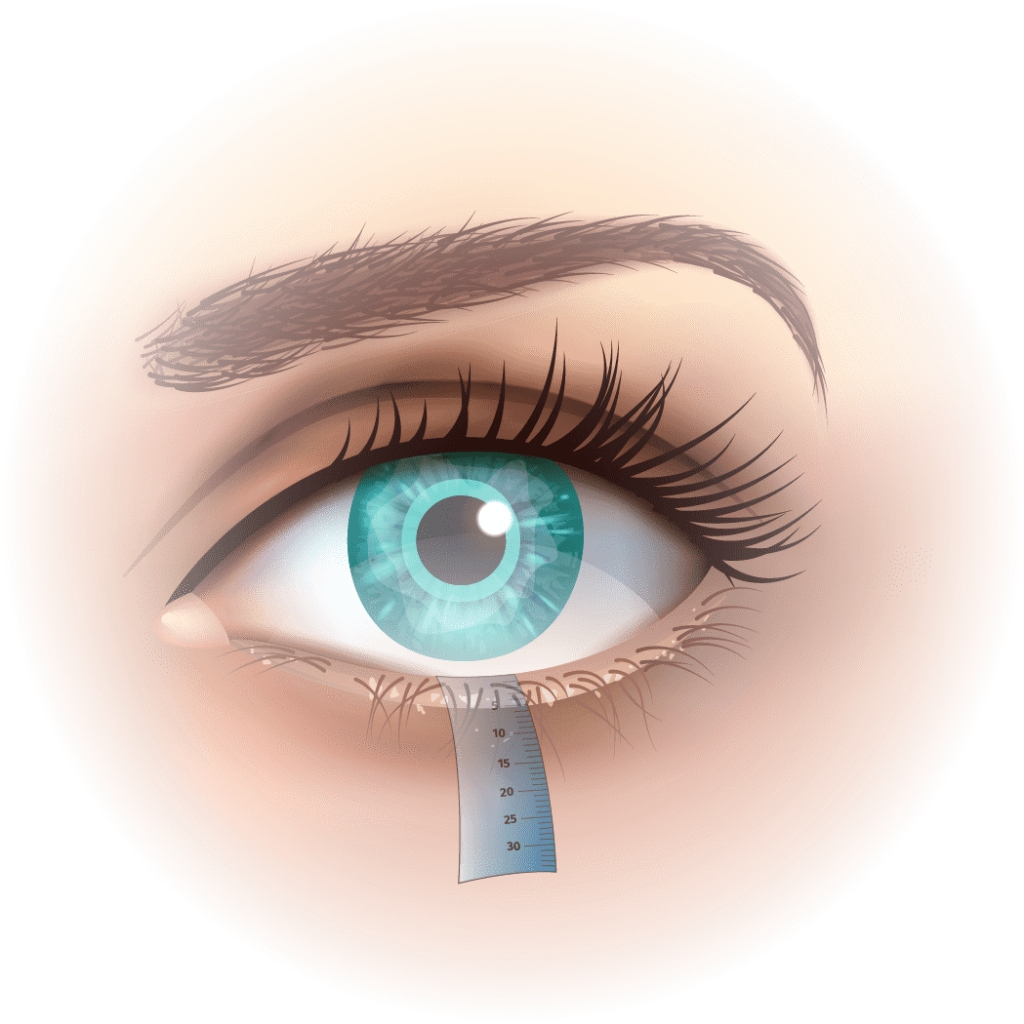
This test measures the amount of tears in the eye using a strip of filter paper placed inside the lower eyelid. It is an invasive method, performed without local anaesthetic. The filter paper gradually soaks up the tears.
If the eye is not producing enough tears, the strip will have less than 10 mm of moisture after five minutes. The test is a quantitative analysis and primarily measures dryness caused by aqueous deficiency, as in Sjögren’s syndrome.

BUT (Break-Up Time)
This test assesses the quality and stability of the tear film on the cornea. A drop of fluorescein is instilled into the patient’s eye. The patient must then stop blinking so that the clinician can measure how long it takes for the tear film—made visible by the fluorescein—to break up. The test is positive if the tear film breaks up after less than 10s.
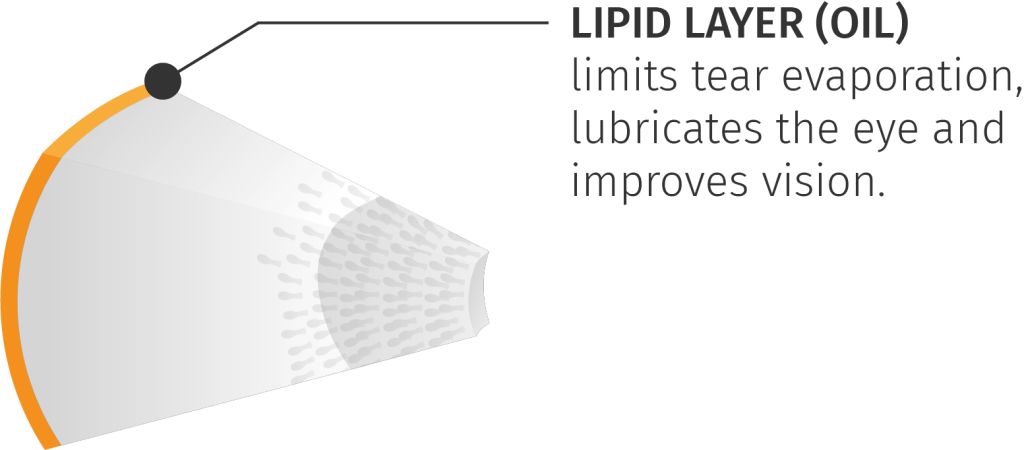
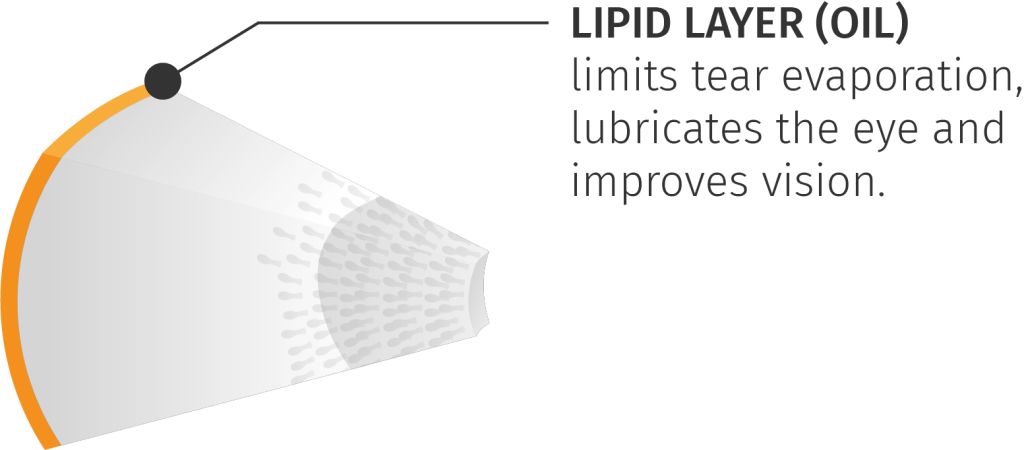
This test generally points to a problem with the lipid layer linked to excessive tear evaporation.

Questionnaire
There are several questionnaires used to assess the severity of dry eye and its impact on patients’ quality of life, including DEQ-5 (Dry Eye Questionnaire), OSDI (Ocular Surface Disease Index) and SPEED (Standard Patient Evaluation of Eye Dryness).
Clinical analysis
It is important to assess the appearance of the skin (for rosacea, eczema, psoriasis, seborrhoeic dermatitis), the anatomy of the eyelids, the appearance of the eyelashes, and blinking frequency.
Schirmer’s test
This test measures the amount of tears in the eye using a strip of filter paper placed inside the lower eyelid. It is an invasive method, performed without local anaesthetic. The filter paper gradually soaks up the tears.
If the eye is not producing enough tears, the strip will have less than 10 mm of moisture after five minutes. The test is a quantitative analysis and primarily measures dryness caused by aqueous deficiency, as in Sjögren’s syndrome.

BUT (Break-Up Time)
This test assesses the quality and stability of the tear film on the cornea. A drop of fluorescein is instilled into the patient’s eye. The patient must then stop blinking so that the clinician can measure how long it takes for the tear film—made visible by the fluorescein—to break up. The test is positive if the tear film breaks up after less than 10s.
This test generally points to a problem with the lipid layer linked to excessive tear evaporation.
New non-contact examinations
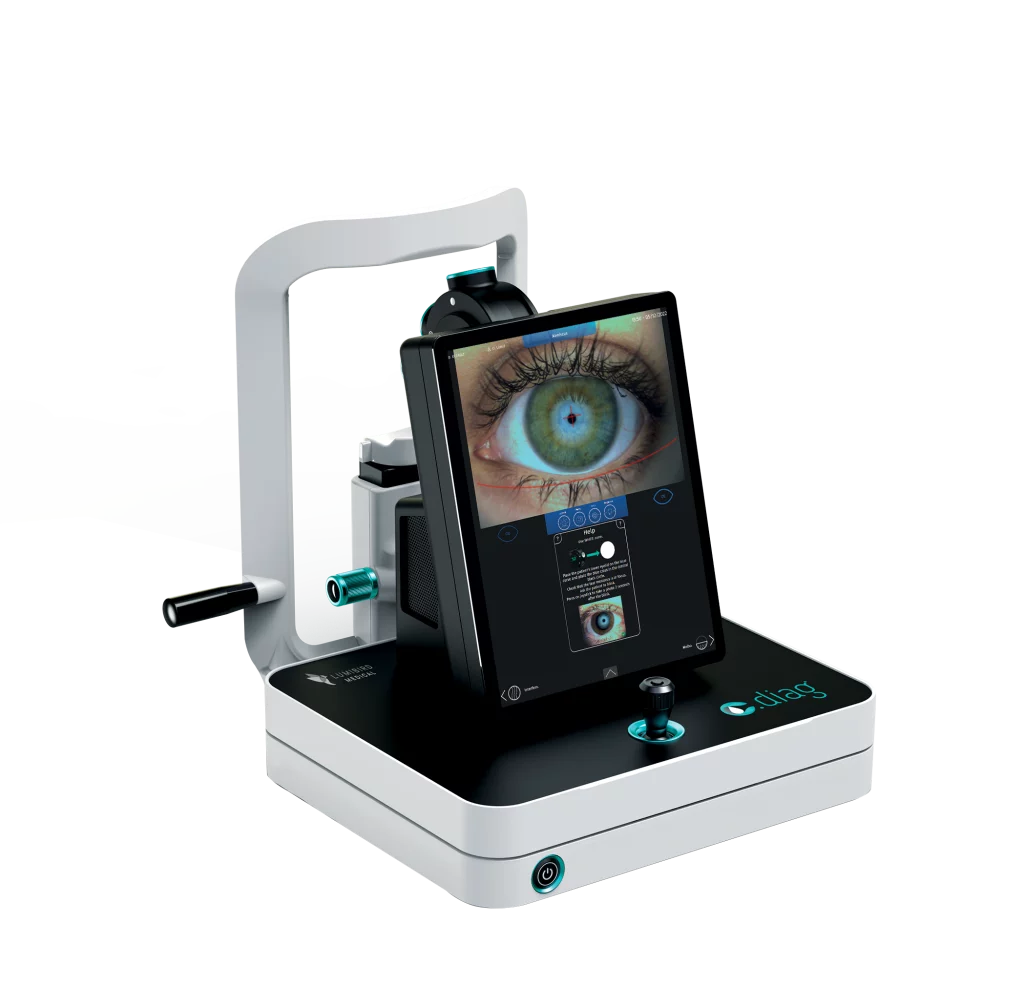
Today, there are an increasing number of imaging devices available to help clinicians better diagnose dry eye and provide patients with more targeted treatments.
New non-contact examinations are now available to assess tear quality and quantity, along with meibomian gland imaging.
The C.DIAG ocular surface analyser can conduct the following tests:
Tear stability
Non-invasive tear film break-up time is used to assess tear stability on the cornea. This test measures how long the tear remains on the cornea after blinking and the point at which it breaks. A stable tear should have a NIBUT of over 10 seconds.
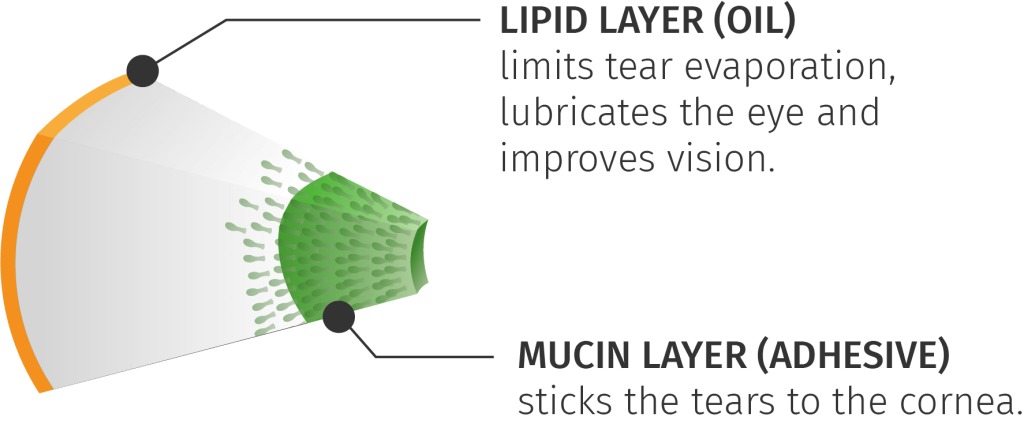
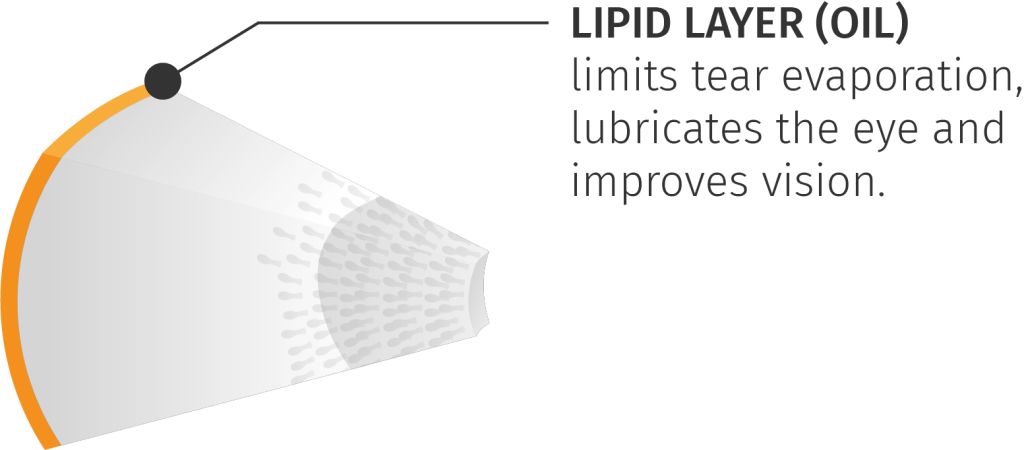
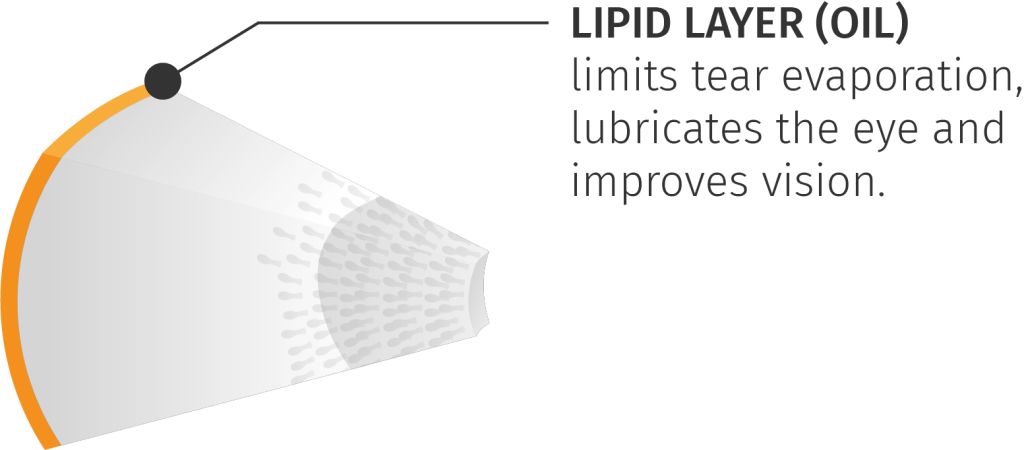
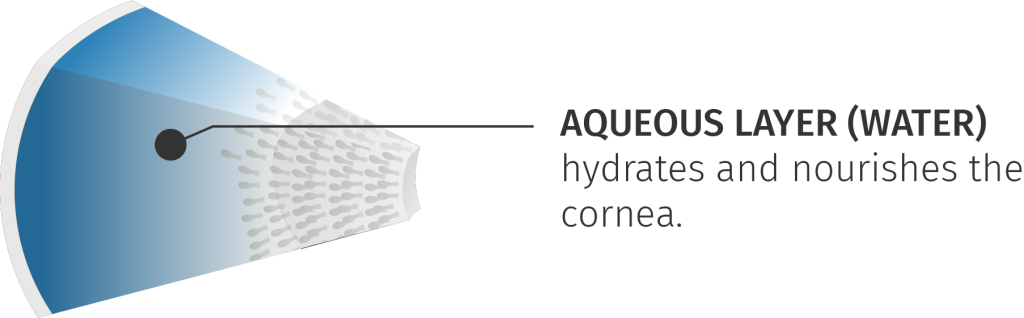
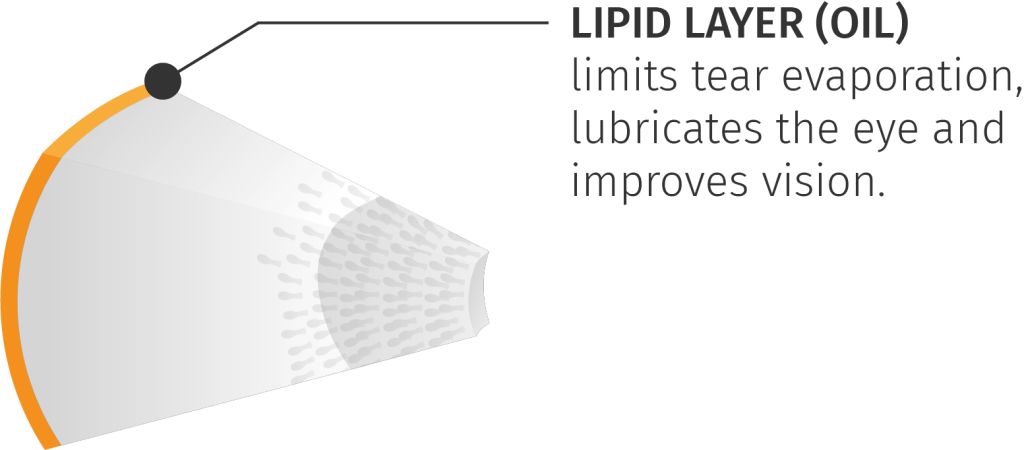
Lipid layer
This examination assesses the thickness of the lipid layer. The colour and structure of the lipid layer (coloured fringes resembling an oil stain) can be examined to determine its quality and thickness. This test is particularly useful for diagnosing meibomian gland dysfunction.
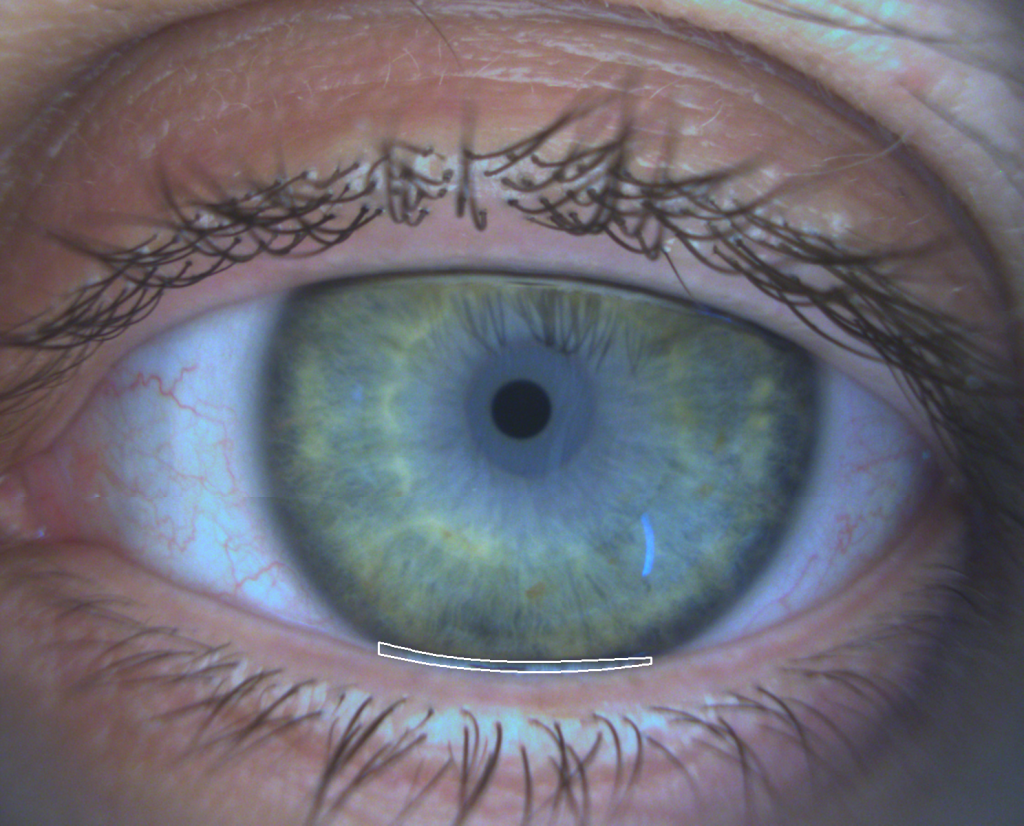
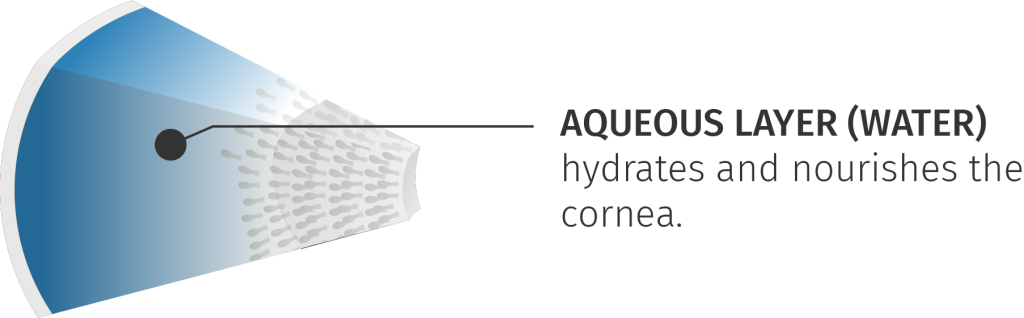
Measurement of tear meniscus height
This examination assesses the amount of water in the tears by measuring the height of the tear meniscus (where the tear meets the edge of the eyelid). If there is no tear meniscus, this indicates dry eye. The normal tear meniscus height is over 0.21 mm.
Meibography
This test quickly provides a complete image showing the shape of the meibomian glands. Meibography is used to assess meibomian gland loss, atrophy and obstruction.

Blinking analysis
This test measures the number of blinks and identifies incomplete blinking. Incomplete blinking often causes meibomian gland dysfunction (MGD), which results in evaporative dry eye due to a thin lipid (oil) layer.
Tear stability
Non-invasive tear film break-up time is used to assess tear stability on the cornea. This test measures how long the tear remains on the cornea after blinking and the point at which it breaks. A stable tear should have a NIBUT of over 10 seconds.
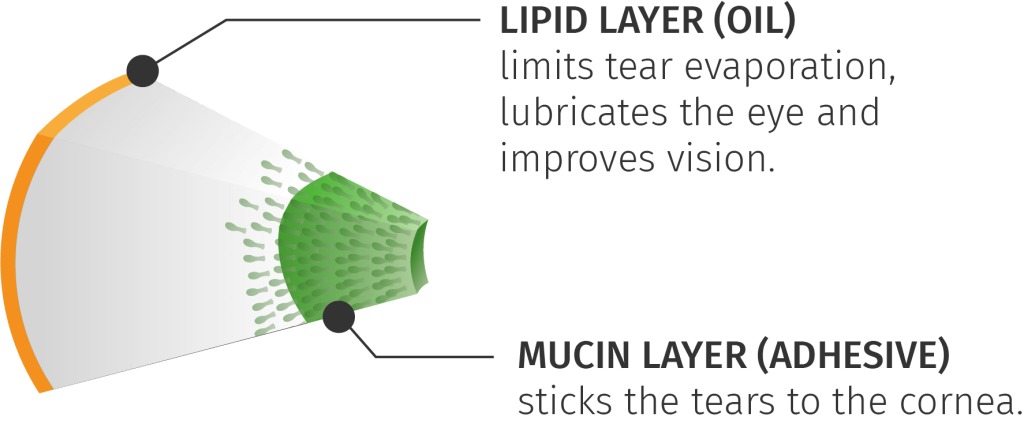
Lipid layer
This examination assesses the thickness of the lipid layer. The colour and structure of the lipid layer (coloured fringes resembling an oil stain) can be examined to determine its quality and thickness. This test is particularly useful for diagnosing meibomian gland dysfunction.
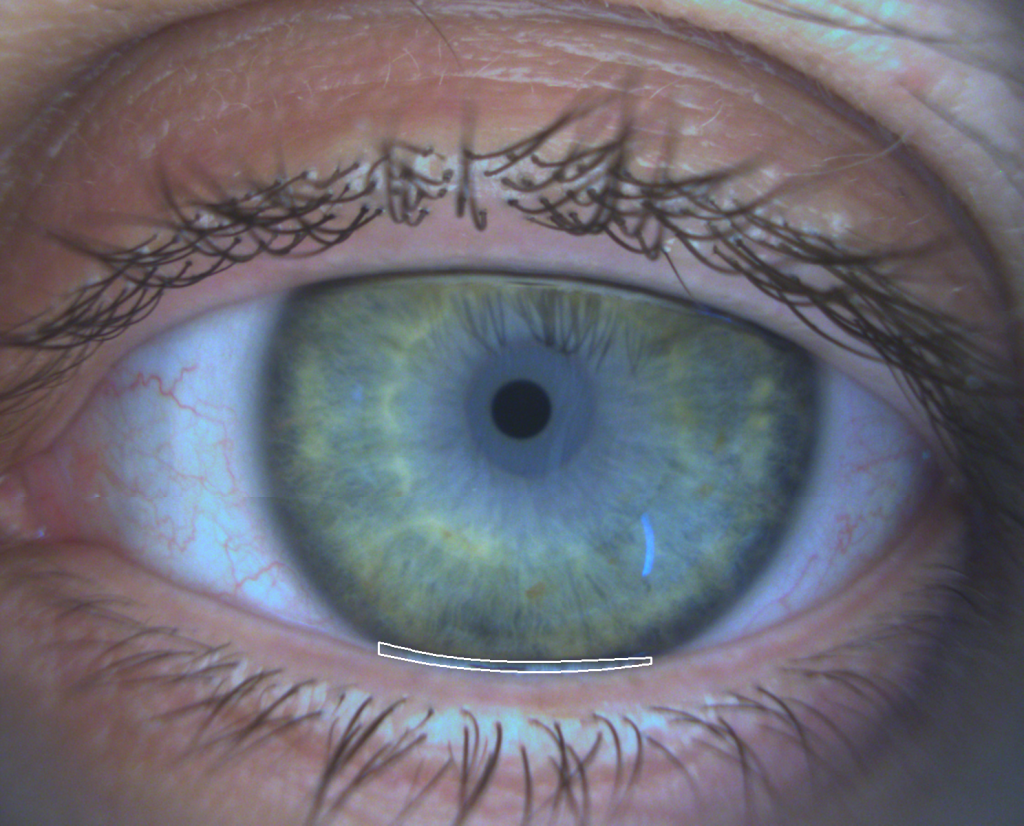
Measurement of tear meniscus height
This examination assesses the amount of water in the tears by measuring the height of the tear meniscus (where the tear meets the edge of the eyelid). If there is no tear meniscus, this indicates dry eye. The normal tear meniscus height is over 0.21 mm.
Meibography
This test quickly provides a complete image showing the shape of the meibomian glands. Meibography is used to assess meibomian gland loss, atrophy and obstruction.

Blinking analysis
This test measures the number of blinks and identifies incomplete blinking. Incomplete blinking often causes meibomian gland dysfunction (MGD), which results in evaporative dry eye due to a thin lipid (oil) layer.
Unsure? Take the test and get your results in a few clicks
Think you may have dry eye? Take two minutes to assess your symptoms using the DEQ-5 questionnaire (five questions) provided on our site.

DEQ-5
A word from the specialists...
Nothing beats the view of a professional, so why not see what our ophthalmologists have to say?

What is dry eye and how is it treated?
New IPL (intense pulsed light) treatments—all completely painless—are now available alongside a range of other treatment options for dry eye. But how much do you know about this disease?

